What is It?
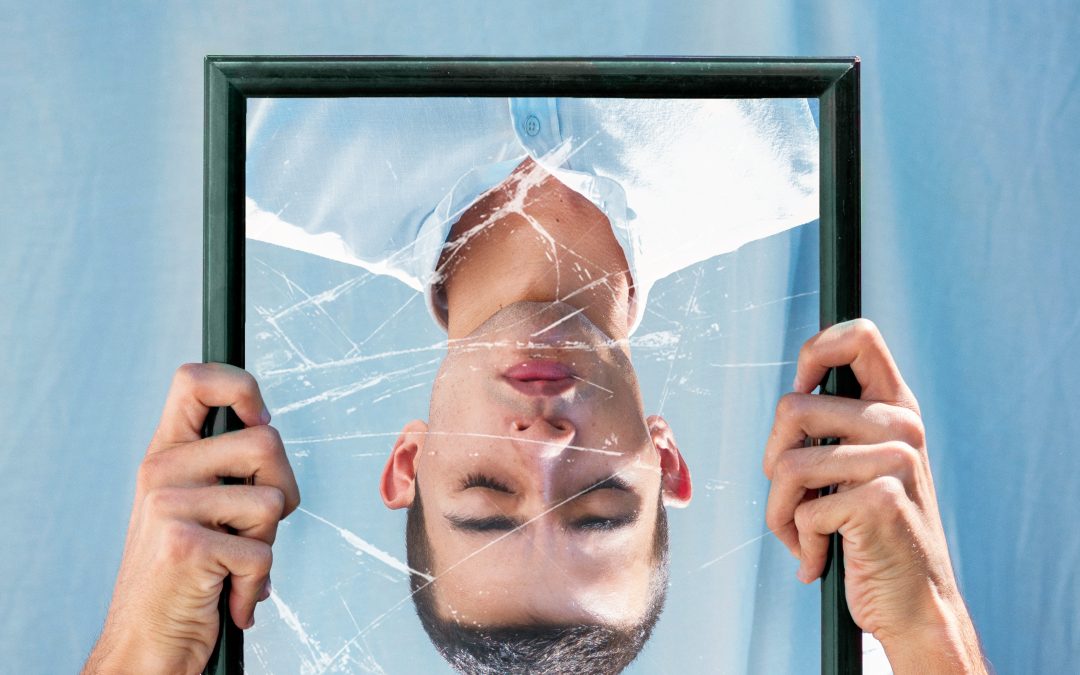
We all have that one imperfection we wish we could change – a crooked tooth, a large nose, acne-prone skin, eyes that are too narrow, a flabby stomach, and the list goes on. However, we accept it and carry on with our daily lives – it’s more of an annoyance than a debilitating thought. If you suffer from body dysmorphic disorder (BDD), you become fixated on that imperfection – obsessed, really – until it becomes the only thing you see when you look in the mirror. These obsessive and controlling thoughts can lead you to spend exorbitant amounts of time trying to cover or conceal the flaw, to seek verbal approval of your looks, even though you are not likely to believe what people tell you, to socially withdraw, and to have thoughts of suicide.
Body dysmorphic disorder, also known as dysmorphophobia, is a common affliction, affecting approximately 1.7% to 2.4% of the population, with roughly equal distribution among men and women. The disorder usually first surfaces in adolescence and is characterized not only by obsessive thinking about a flaw that is usually imagined or if present, hardly noticeable to the general population, but also characterized by compulsive checking of the perceived flaw (for example, spending lots of time in front of the mirror), engaging in behaviors to minimize the appearance of the perceived flaw (i.e., covering it up with makeup or an article of clothing), and hiding the disorder from others due to fear of social stigma. Whereas most individuals might be annoyed by a real or imagined physical imperfection, if you are suffering from body dysmorphic disorder, you are likely spending hours and hours a day obsessing over it, taking excessive precautions to hide from others (i.e., social isolation) so others will not notice the perceived flaw, exercising excessively, and even undergoing drastic plastic surgery to try to “fix” the flaw, usually with non-satisfactory results. The most common places you are likely to perceive a flaw if you are suffering from BDD is your hair, skin, stomach, nose, or chest. Although the most common, this list is not exhaustive and a perceived flaw can happen anywhere on the body.
Body dysmorphic disorder is similar to both obsessive-compulsive disorder and eating disorders, but presents itself slightly differently. If you have an eating disorder, you are preoccupied by your overall weight and body shape, where if you suffer from body dysmorphic disorder, you are preoccupied with one specific body part. With obsessive-compulsive disorder, you may suffer from recurrent thoughts, fears, or images you have no control over. The anxiety that results from these thoughts usually leads to the performance of rituals or routines (known as compulsions). When you have BDD, the obsession with the perceived flaw or defect leads to ritualistic behaviors (e.g., skin picking) and the obsession over the flaw leads to social, work, or home functioning impairment. One study found that 24% of individuals with BDD also suffered from obsessive-compulsive disorder.
What are the Symptoms?
There are many signs and symptoms of body dysmorphic disorder – and they widely vary from person to person. As mentioned above, if you are suffering from BDD, you likely spend an excessive amount of time obsessing over a perceived flaw on a specific body part. Then, compulsively exhibit any number of behaviors to try to rid yourself of the defect.
If you are experiencing BDD, some of the most common body parts that you may fixate on are:
- Moles and freckles (especially related to their size – too large or too noticeable)
- Minor scars or aberrations
- Acne
- Facial and body hair
- Too little hair on head (e.g., balding or hair thinning)
- Size and shape of genitalia
- Size of breasts
- Muscle size (belief that the muscles are too small – also known as muscular dysmorphia)
- Size, shape, and/or symmetry of the face or another body part
Individuals with BDD are likely to exhibit one or many of the following behaviors or compulsions:
- Repetitive checking of a real or imagined flaw in the mirror
- Avoidance of mirrors
- Avoidance of having your picture taken
- Repetitive grooming activities (e.g., combing hair, shaving)
- Repetitive touching, checking, or measuring perceived flaw (minor or imagined)
- Wearing excessive makeup or growing a beard to cover up perceived flaw (minor or imagined)
- Wearing certain types of clothing (e.g., hats, scarves) to cover up perceived flaw (minor or imagined)
- Making multiple doctor visits, especially to dermatologists
- Undergoing multiple medical procedures (e.g., plastic surgeries) to try to eradicate or minimize the perceived flaw (minor or imagined) – usually resulting in unsatisfactory results
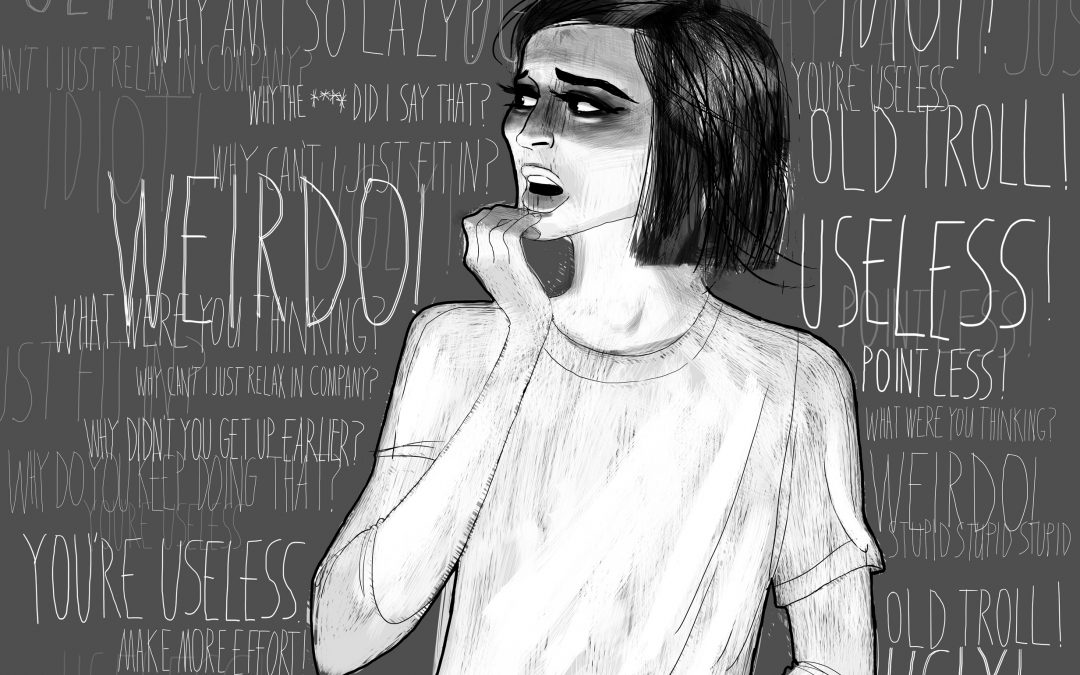
- Frequent thoughts about your appearance (hours per day)
- Repeatedly asking others for their verbal opinion of how you look (i.e., reassurance seeking) – not believing them when they say you look great
- Compulsive skin picking, using fingernails or tweezer to remove unwanted hair or blemishes
- Leaving the house less often or only going out at night to try to camouflage your appearance in the darkness
- Keeping obsessions and compulsions secret for fear of social stigma
- Emotional problems, including depression, feelings of disgust, low self-esteem, and anxiety
- Avoidance of social situations
- Belief that others take special notice of your perceived flaw in a negative way
- Excessive exercise
- Changing clothes frequently and excessively
How is it Diagnosed and What Causes It?
Unfortunately, body dysmorphic disorder is not high on many general practitioners’ and other clinicians’ radars and may go undiagnosed or unnoticed. This is especially true since most individuals with BDD hide their obsessions and compulsions from the general public so well. Often times, body dysmorphia is misdiagnosed as social phobia or major depressive disorder. One red flag though is repetitive plastic surgery for the same or multiple perceived physical defects. A trained clinician will diagnose BDD – beginning with a health history and a physical exam. If body dysmorphic disorder is suspected, you are likely to be sent to a mental health professional who will make a diagnosis based on his or her assessment of your attitude, behaviors, and symptoms.
So, you have been diagnosed with body dysmorphic disorder. You may be asking yourself, how did I end up with this? What caused it? All very good and likely questions. Mental health professionals and researchers have not found the one specific cause of BDD. But, they point out that like many other mental health disorders, it’s likely due to a number of causes. Brain differences, genes, and the environment are the likely culprits. Your risks of having to cope with BDD are heightened if you have biological relatives with BDD, experienced negative childhood situations (e.g., bullying or teasing), exhibit certain personality traits, such as low self-esteem, experience societal pressures to be “pretty” or “beautiful,” and if you suffer from another psychiatric disorder, such as anxiety or depression.
How is it Treated?
The two most common treatment options for body dysmorphic disorder is medication and therapy. Cognitive behavioral therapy has been found to be the most effective at treating BDD and a certain type of antidepressants have also been shown to help individuals coping with the disorder.
Cognitive behavioral therapy is a coping technique that teaches individuals suffering from body dysmorphia how to recognize irrational thoughts and change negative thinking patterns. You then are instructed on how to take those negative thoughts and replace them with positive ones. Exposure and response prevention are two key processes involved in cognitive-behavioral therapy. Exposure helps individuals experiencing BDD confront situations that cause irrational fear (e.g., going out in public with the perceived flaw uncovered). Response prevention teaches you how to resist the urge to cover up your perceived flaw with makeup or clothing, how to stop seeking reassurance from others about your appearance, and how to decrease time spent repeatedly checking your appearance.
Antidepressants, more specifically, selective serotonin reuptake inhibitors (SSRIs) can also be prescribed to individuals living with body dysmorphic disorder as they help relieve the obsessive and compulsive thoughts and behaviors associated with the disorder. These are effective, in part, because it is believed that a partial cause of body dysmorphia is due to problems related to the brain chemical serotonin. Your doctor may prescribe you a gradual dose of antidepressants to make sure you tolerate the medication and the potential side effects. In some situations, you may also be prescribed an antipsychotic drug in addition to an antidepressant, especially if you are experiencing delusions related to your BDD diagnosis.
To get the most out of treatment, be sure to do the following:
- Don’t skip any therapy sessions, even if you don’t feel like talking
- Take your medication as directed – even if you feel fine – there is a chance that your symptoms may return once you stop taking the medication and you could even experience withdrawal symptoms if you stop taking your medication suddenly
- Educate yourself about your condition – learn all you can about the disorder and how it affects your body
- Pay attention to warning signs and certain triggers that enhance your symptoms – speak about these with your therapist and doctor
- Be more active – physical activity can help ease many of the symptoms associated with body dysmorphic disorder, including anxiety and depression
- Avoid drugs and alcohol – they can interact with your medication and worsen mental illness symptoms
- Don’t skip regular, routine health checkups
Source: https://www.psycom.net/eating-disorders/body-dysmorphic-disorder